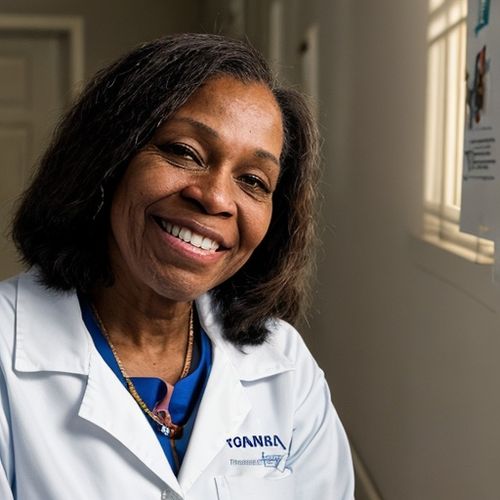
In the annals of medical history, few advancements have captured the imagination and hope of the scientific community as much as xenotransplantation—the practice of transplanting animal organs into humans. Recently, a remarkable story emerged from this pioneering field, highlighting both the promise and the challenges that lie ahead. Towana Looney, a 53-year-old woman from Alabama, made headlines when she lived for 130 days with a genetically engineered pig kidney, the longest any human has ever survived with an animal organ. Her journey is not just a testament to personal bravery but also a significant milestone in the burgeoning field of xenotransplantation.
A Life Changed by Xenotransplantation
Towana Looney’s story is one of resilience and hope. For nine years, she had been on dialysis, a grueling and life-altering procedure that filters waste from the blood when kidneys fail. In late November, Looney became only the third person to receive a kidney from a gene-edited pig while alive. This groundbreaking procedure was performed at the NYU Langone Transplant Institute, a leading center in the field of organ transplantation.
Looney’s decision to undergo the experimental procedure was driven by desperation and hope. After donating a kidney to save her mother’s life in 1999, she later developed kidney failure due to preeclampsia, a serious pregnancy complication. Despite years on the organ transplant waitlist, a suitable human donor remained elusive. When the opportunity to receive a genetically engineered pig kidney presented itself, Looney seized it, supported by her husband and family.
The initial results were promising. Looney left the hospital just 11 days after the surgery and stayed in an apartment near the hospital for daily checkups. For over four months, she enjoyed a life free from the constraints of dialysis, a period she described as transformative. “For the first time since 2016, I enjoyed time with friends and family without planning around dialysis treatments,” she said in a statement. Her experience was a beacon of hope for the thousands of patients awaiting organ transplants.
The Challenges of Xenotransplantation
Despite the initial success, complications eventually arose. In early April, Looney experienced a reduction in renal function due to acute rejection. The trigger for this rejection episode is still under investigation, but it followed a reduction in her immunosuppression regimen, which was necessary to treat an unrelated infection. Dr. Robert Montgomery, director of the NYU Langone Transplant Institute, explained that the decision to remove the kidney was made to preserve future transplantation possibilities for Looney as medical knowledge and innovations continue to progress.
The case underscores one of the biggest challenges in xenotransplantation: balancing the prevention and management of infections with the necessary immunosuppression to prevent organ rejection. United Therapeutics Corporation, the biotech company that developed the modified pig kidney known as a UKidney, acknowledged this delicate balance. They stated that current evidence suggests the UKidney functioned well until the rejection episode, which appears to have been triggered by the reduction in immunosuppression while treating the unrelated infection.
The Promise of Xenotransplantation
Looney’s experience, while not the desired outcome, has provided invaluable insights into the potential and challenges of xenotransplantation. The field holds immense promise, especially given the dire shortage of human organs for transplantation. According to the Organ Procurement and Transplantation Network, over 90,000 people in the United States are on the waitlist for a kidney transplant. The average wait time is three to five years, and approximately 13 people die each day while waiting. Dialysis, while life-sustaining, is far from a perfect solution, offering only 10% to 15% of the functionality of a healthy kidney and resulting in a 50% mortality rate within five years of starting treatment.
The US Food and Drug Administration (FDA) has recognized the potential of xenotransplantation, allowing doctors to transplant pig organs into humans under “compassionate use” regulations. Pigs are particularly suitable for this purpose due to the similarity of their organs to human organs and their rapid reproduction rate. Scientists can further enhance the compatibility of pig organs through genetic editing, reducing the risk of rejection.
Looney was the first recipient of a kidney with 10 gene edits, a significant advancement in the field. United Therapeutics announced in February that it had received FDA clearance to use this type of pig kidney in the first human clinical trials. The company plans to perform the first of six initial transplants in mid-2025, with the goal of expanding the trial to 50 patients. Some experts predict that pig kidney transplants could become a standard option for patients within a decade, a development that would revolutionize organ transplantation.
Towana Looney’s Enduring Impact
Despite the eventual removal of the pig kidney, Towana Looney’s journey has left an indelible mark on the field of xenotransplantation. Her willingness to take a leap into the unknown has provided critical data and insights that will benefit countless patients in the future. Dr. Montgomery celebrated her bravery, stating, “Towana’s willingness to endeavor into the unknown to help solve the nation’s organ shortage crisis will impact many more lives after her. We celebrate her tremendous courage and sacrifice.”
United Therapeutics echoed this sentiment, emphasizing that Looney’s case will continue to contribute to the scientific community’s understanding of xenotransplantation. Her experience, from the initial transplant procedure to the post-transplant management of the xenograft, offers valuable lessons for researchers and clinicians alike.
Looney’s story is a poignant reminder of the human cost of organ shortages and the urgent need for innovative solutions. Her bravery has not only advanced the field of xenotransplantation but also inspired hope for those facing similar challenges. As researchers and clinicians continue to push the boundaries of medical science, Looney’s legacy will remain a testament to the power of human resilience and the potential of groundbreaking medical advancements.
Looking Ahead
The future of xenotransplantation holds both promise and challenges. While Looney’s experience highlights the complexities of balancing immunosuppression and infection management, it also underscores the potential for genetically engineered pig organs to alleviate the organ shortage crisis. As clinical trials progress and more data become available, the scientific community will continue to refine and improve xenotransplantation techniques.
The journey of Towana Looney serves as a powerful reminder of the importance of supporting research and innovation in medicine. Her story is not just about a single patient’s experience but about the collective hope for a future where organ shortages are a thing of the past. As we celebrate her bravery and contributions, we must also recognize the ongoing efforts of researchers, clinicians, and patients who are pushing the boundaries of what is possible in organ transplantation.
In the end, Towana Looney’s legacy is one of hope, resilience, and progress. Her 130 days with a pig kidney have taught us much about the potential of xenotransplantation and have inspired countless others to continue the fight against kidney disease. As we look to the future, her story will remain a beacon of hope for all those awaiting a life-changing transplant.

By Samuel Cooper/Apr 16, 2025

By James Moore/Apr 16, 2025
By Sophia Lewis/Apr 16, 2025

By Michael Brown/Apr 16, 2025

By Christopher Harris/Apr 16, 2025

By Natalie Campbell/Apr 16, 2025

By George Bailey/Apr 16, 2025

By Thomas Roberts/Apr 16, 2025

By Natalie Campbell/Apr 16, 2025

By John Smith/Apr 16, 2025

By Emma Thompson/Apr 15, 2025

By Lily Simpson/Apr 15, 2025

By Noah Bell/Apr 15, 2025

By Victoria Gonzalez/Apr 15, 2025

By Benjamin Evans/Apr 15, 2025

By Joshua Howard/Apr 15, 2025

By Daniel Scott/Apr 15, 2025
By Amanda Phillips/Apr 15, 2025

By James Moore/Apr 15, 2025

By Grace Cox/Apr 15, 2025